SMALLPOX VACCINE
The history of smallpox holds a unique place in medicine. It was one of the deadliest diseases known to humans, and to date (2016) the only human disease to have been eradicated by vaccination. The smallpox vaccine, introduced by Edward Jenner in 1796, was the first successful vaccine to be developed. He observed that milkmaids who previously had caught cowpox did not catch smallpox and showed that inoculated vaccinia protected against inoculated variola virus.
The global eradication effort initially used a strategy of mass vaccination campaigns to achieve 80% vaccine coverage in each country, and thereafter by case-finding, followed by ring vaccination of all known and possible contacts to seal off the outbreak from the rest of the population.
In 1961 the bifurcated needle was developed as a more efficient and cost effective alternative, and was the primary instrument used during the eradication campaign from 1966 to 1977. The bifurcated needle vaccination required only one-fourth the amount of vaccine needed with previous methods and was simpler to perform.
Different types of vaccine
Smallpox vaccines produced and successfully used during the intensified eradication program are called first generation vaccines in contrast to smallpox vaccines developed at the end of the eradication phase or thereafter and produced by modern cell culture techniques. Second generation smallpox vaccines use the same smallpox vaccine strains employed for manufacture of first generation vaccines or clonal virus variants plaque purified from traditional vaccine stocks, whereas third generation smallpox vaccines represent more attenuated vaccine strains specifically developed as safer vaccines at the end of the eradication phase by further passage in cell culture or animals. Second and third generation vaccines are produced using modern cell culture techniques and current standards of Good Manufacturing Practices (GMP).
The need for WHO to maintain an emergency reserve of smallpox vaccine following eradication was recognized in 1980 when WHO was given a set of formal responsibilities for maintaining capacity and expertise to respond to a re-emergence of smallpox in the post-eradication era as both a component of a preparedness strategy and a possible deterrent to intentional release. The Smallpox Vaccine Emergency Stockpile (SVES) was originally created by consolidating WHO Member State donations given in support of the Intensified Smallpox Eradication Programme.
In 2002, World Health Assembly (WHA) Resolution 55.16 urged Member States to share expertise, supplies and resources to rapidly contain a public health emergency or mitigate its effects. The resolution further requested the WHO Director General to examine the possible development of collaborative mechanisms to prepare and stockpile resources for a potential PHEIC. The SVES currently consists of two components:
A physical stockpile of vaccine held by WHO Headquarters in Switzerland, which is composed of calf-lymph smallpox vaccines from a variety of sources dating from the final years of the eradication program that are regularly tested for potency. It is estimated to consist of approximately 2.4 million doses when reconstituted and delivered by bifurcated needle.
A pledged stockpile held by Donor countries in their respective national stockpiles for use in time of international need upon request by WHO, which currently consists of 31.01 million doses of smallpox vaccine held by France, Germany, Japan, New Zealand, and the United States.
SAGE
Given the different set of vaccines available (1st generation vaccines used during the eradication campaign and made from the lymph or skin of inoculated animals, 2nd generation vaccines produced in tissue cells and further attenuated, and 3rd generation vaccines based on replicating or non-replicating virus) WHO needs to be able to make an informed decision on which vaccines to include in the stockpile for use in case of a re-emergence of smallpox. Therefore, Strategic Advisory Group of Experts on immunization (SAGE) was asked to respond to the following questions: Which vaccine should be recommended for use during an outbreak of smallpox and how many doses should be stockpiled? What groups should be targeted for vaccination if an outbreak occurs? Which groups should be vaccinated for preventive use and with which vaccine?
- Meeting of the Strategic Advisory Group of Experts on immunization, conclusions and recommendations
3 January 2014
GACVS
The Global Advisory Committee on Vaccine Safety (GACVS) was requested to review the safety of smallpox vaccination. The Committee was provided with updated safety information for 1st, 2nd and 3rd generation smallpox vaccines in order to make informed decisions regarding emergency smallpox vaccine stockpiling and future use. The safety update also included an overview of the safety of smallpox vaccines used in the smallpox eradication efforts.
- Global Advisory Committee on Vaccine Safety
2-3 December 2015 - Safety of smallpox vaccines
WHO Smallpox Vaccine Emergency Stockpile
This document describes the WHO Smallpox Vaccine Emergency Stockpile (SVES) and the considerations and processes needed for countries to request vaccine in the event of a smallpox outbreak.
HISTORY OF SMALLPOX VACCINATION AND GLOBAL ERADICATION
Smallpox has been a scourge against humanity for at least the past 1500 years, and perhaps much longer than that. There is no mention of the disease in ancient Greek writings, but plagues of pustular disease in the Roman Empire bore a strong resemblance to smallpox. The literary record suggests that smallpox became established in the Mediterranean by the third century AD, and it was described in China around the same time.1 Smallpox subsequently changed the course of history and killed millions of people in both the New World and the Old World.
Smallpox is caused by the variola virus, a DNA virus of the genus Orthopoxvirus. Humans are the only known reservoir for this virus. It is transmitted from person to person, and natural infection occurs by inhalation of respiratory droplets or contact with infected material on mucous membranes. Historical data suggest that smallpox is not highly transmissible, and high population densities are required to sustain transmission. Persons who have close, prolonged contact with an infected patient are at highest risk.2 After a 10 to 14 day incubation period, the infected person develops severe symptoms with fever, malaise and headache.3 A maculopapular rash then develops with involvement of the face, mucous membranes, trunk and extremities. The lesions become pustular and deep over the subsequent 1 to 2 days, with scab formation by day 10. Patients are most infectious during the first week of the rash when viral shedding is greatest from ulcerated lesions in the oral mucosa. The overall mortality rate is about 30%, with most deaths occurring during the second week of illness.
The earliest smallpox prevention efforts date back to at least the 10th century in China, when physicians found that nasal inoculation of susceptible persons with material from smallpox lesions would sometimes provide immunity.4 The practice of inoculation appears to have arisen independently in several other regions prior to the 17th century, including Africa and India, but the practice did not gain popularity in western Europe until the 18th century. The wife of an English ambassador, Lady Montagu, observed inoculation in Turkey, and later had her own child successfully inoculated during a smallpox epidemic in England.5 In this procedure a lancet or needle was used to deliver a subcutaneous dose of smallpox material to a susceptible person. The procedure, also known as variolation, was controversial. It generated immunity in many cases, but it also killed some people and contributed to smallpox outbreaks.
A more safe and effective method for smallpox control originated in the late 18th century when Dr. Edward Jenner of Gloucestershire, England noticed that milkmaids exposed to cowpox appeared to be immune to smallpox. He tested his hypothesis by inoculating a boy with cowpox pus and subsequently challenging him with smallpox. The experiment was a success, and Jenner prepared a paper describing this case along with 13 other individuals who had contracted either horsepox or cowpox before being exposed to smallpox. In one of the worst editorial decisions of all time, the Royal Society rejected the paper and suggested that Jenner cease his cowpox investigations.5 Jenner wisely ignored this advice, named the cowpox material the “vaccine virus”, and thus discovered the concept of vaccination.1, 6 Early smallpox vaccinations utilized pustular material from one vaccinated person to directly inoculate another person by scratching the material into the recipient's arm. Later improvements included the inoculation of cow flanks to obtain larger quantities of virus, and use of glycerol solution as a preservative.7 A textbook published in the early 20th century described the vaccination process as follows:
A spot, usually on the upper arm, is scraped by a lancet, so that the outer layers of the epidermis are removed; the spot is then rubbed with an ivory point, quill or tube, carrying the virus. A slight and usually unimportant illness or indisposition follows, and the arm is sore for a time, a characteristic scar remaining.8
The modern vaccine was conceived in the 1950s when a technique was developed to produce a heat-stable, freeze-dried vaccine. This process used centrifugation to create a suspension of virus, which was then freeze-dried in ampules. This had the advantage of allowing long-term storage without refrigeration.
The first large smallpox eradication effort was launched in 1950 with the goal of eliminating smallpox in the Americas. In 1958, the World Health Assembly passed a resolution calling for the global eradication of smallpox. Although some countries established smallpox eradication programs, there was no coordinated infrastructure. Many programs faltered due to insufficient vaccine supplies and limited resources.
The more virulent form of smallpox, variola major, was widespread in the United States during the 19th century, but only two major outbreaks occurred from 1900 to 1925.9 In contrast, the milder form of smallpox (variola minor) was common until the 1930s. After 1949, there were no endemic cases of smallpox in the United States, but the disease continued to be a serious problem in less developed countries. By 1966, smallpox remained endemic in 33 countries.7 After extensive debate, the World Health Assembly approved $2.4 million to initiate a global eradication program over the next 10 years. Early in the campaign the Soviet Union and the United States donated more than 150 million doses of vaccine. Around the same time, the bifurcated needle was developed, which simplified delivery and reduced the volume of vaccine required.
The global eradication effort, led by D.A. Henderson, originally used a strategy of mass vaccination campaigns to achieve 80% vaccine coverage in each country. This goal proved difficult to attain in many underdeveloped countries, but a serendipitous discovery led to a more effective strategy. Insufficient vaccine supplies in Nigeria led Dr. William Foege to try a strategy of aggressive case-finding, followed by vaccination of all known and possible contacts to seal off the outbreak from the rest of the population.5 This was the first time such a strategy was employed during the global smallpox eradication campaign, although it was also used in Leicester, England in the late 19th century.9 This strategy, known as surveillance-containment or ring vaccination, led to the disappearance of smallpox in eastern Nigeria even though the population coverage was less than 50%. The relative benefits of ring vaccination versus mass vaccination have been debated, but epidemiological evidence from Africa and Asia suggests that both lower population density and higher population vaccine coverage contributed to the elimination of transmission in many regions.10
The last naturally-acquired case of the variola major was identified in Bangladesh in late 1975. The last case of illness caused by the less virulent strain (variola minor) occurred in Somalia in 1977.5,11 The World Health Assembly declared that smallpox had been eradicated from the earth in 1980. Although the significance of this event may be under appreciated, it stands as one of the greatest accomplishments of the 20th century, if not one of the greatest human accomplishments of all time. Several factors unique to smallpox contributed to the success of this effort, including easily-diagnosed clinical disease, lack of subclinical infections, absence of transmission during prodrome, and lack of an animal reservoir.12
In 1976, the World Health Organization requested that all laboratories with smallpox virus either destroy the virus or submit their stocks to one of two collaborating centers in the United States (Centers for Disease Control) or the Soviet Union (Moscow Institute). Most laboratories complied, but there is evidence that smallpox was subsequently developed as a biological weapon in the Soviet Union.6 Large volumes of weaponized smallpox virus may be unaccounted for, and there is concern that smallpox stocks may have been acquired by other nations. There have also been allegations that Russia has developed recombinant strains of smallpox with increased virulence and infectivity.3 These concerns have contributed to the current interest in renewed smallpox vaccinations, particularly since the September 11, 2001 terrorist attack and the use of anthrax as a biological weapon later in 2001.
SMALLPOX VACCINE
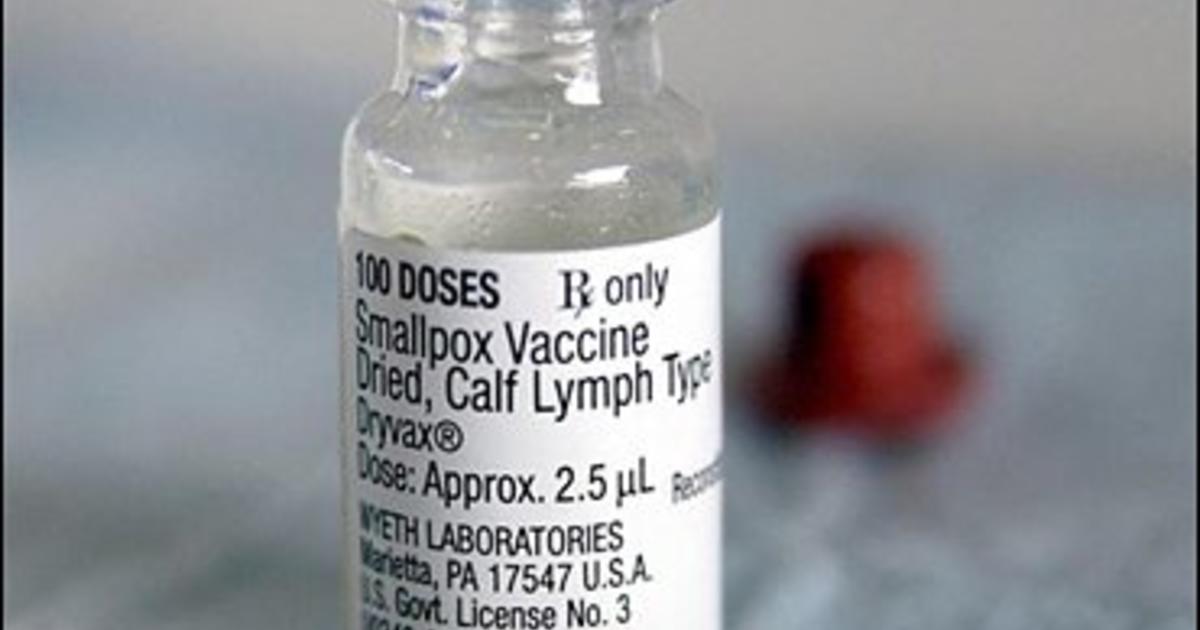
The most widely used virus for smallpox inoculation has been vaccinia, which belongs to the genus Orthopoxvirus along with variola virus. Other species of Orthopoxvirus include cowpox (the virus used by Jenner), monkeypox, and camelpox, among others. Vaccinia is a double-stranded DNA virus with a wide host range. Its origin is uncertain, and there are many strains of vaccinia with different biological properties.9 Vaccinia induces both cellular and humoral immunity to variola virus.13 The current U.S. licensed smallpox vaccine (Dryvax, Wyeth Laboratories, Inc.) was prepared from calf lymph using the New York City Board of Health (NYCBOH) strain of vaccinia. Production of this vaccine was discontinued in 1982. The National Pharmaceutical Stockpile also includes the Aventis Pasteur vaccine, which was also manufactured from calf lymph. Multiple other strains of vaccinia have been used in other regions the world.
Long-term research is underway using recombinant DNA technology to develop a safer vaccine that will provide an effective immune response without replication of vaccinia virus.14 Two companies are currently funded by the United States government to develop and test a vaccine based on the modified Ankara strain of vaccinia, which is nonreplicating in mammalian cells (Washington Post, February 26, 2003). In the short term, two new, unlicensed smallpox vaccines have been developed by Acambis/Baxter Pharmaceuticals. Both use the NYCBOH strain of vaccinia virus, but one is cultured from human embryonic lung cell culture and the other uses African green monkey (vero) cells.15 At this time it is not known if these vaccines will be more or less reactogenic than the current calf-lymph derived vaccine. Clinical trials are underway. Until a new vaccine is licensed by the U.S. Food and Drug Administration, existing doses of Dryvax can be diluted 1:10 and still generate an adequate immune response if the number of required vaccinations exceeds the number of doses in the national stockpile.16
Effective smallpox vaccines have a vaccinia titer of approximately 108 pock-forming units per mL, and more than 95% of individuals develop a ‘take’ with neutralizing antibodies after primary vaccination.13 The efficacy of the vaccine has not been evaluated in controlled studies, but epidemiologic data suggest that a high level of protection persists for up to 5 years after vaccination, with partial immunity persisting for 10 years or more.11 The vaccine will prevent infection or reduce the severity of illness if given within a few days following exposure to smallpox.3
Smallpox vaccine is administered by puncturing the skin multiple times with a bifurcated needle containing a small quantity of vaccine. A small papule develops after 3 to 5 days, following the virus replication in the dermis. The papule evolves into a vesicular and pustular stage over 8 to 10 days.17 There is typically an indurated area surrounding the central lesion. This is followed by scab formation with development of a residual scar. The process of vesiculation and pustule formation defines a ‘take’ of the vaccine. The take is considered equivocal if a pustule, ulcer, or scab, does not develop at the vaccine site; revaccination is recommended in this situation.17 Skin reactions following revaccination tend to be milder and have an accelerated course.
ADVERSE EFFECTS OF VACCINATION
Frequency and Clinical Features
Smallpox vaccine is less safe than other vaccines routinely used today. The vaccine is associated with known adverse effects that range from mild to severe. Mild vaccine reactions include formation of satellite lesions, fever, muscle aches, regional lymphadenopathy, fatigue, headache, nausea, rashes, and soreness at the vaccination site.13,18,19 A recent clinical trial reported that more than one-third of vaccine recipients missed days of work or school because of these mild vaccine-related symptoms.18
In the 1960s, serious adverse events associated with smallpox vaccination in the United States included death (1/million vaccinations), progressive vaccinia (1.5/million vaccinations), eczema vaccinatum (39/million vaccinations), postvaccinial encephalitis (12/million vaccinations), and generalized vaccinia (241/million vaccinations).20 Adverse events were approximately ten times more common among those vaccinated for the first time compared to revaccinees.20 Fatality rates were also four times higher for primary vaccinees compared to revaccinees.21
Inadvertent inoculation is the most common adverse event associated with smallpox vaccination. It occurred at a rate of 529 per million vaccinations in a 1968 study.20 Inadvertent or accidental inoculation usually occurs when a person transfers the vaccinia virus from the vaccination site to another location on their body, usually the eyes, mouth, nose, or genitalia.20,22 Most lesions resolve without therapy, but vaccinia immune globulin (VIG) may be useful for difficult lesions. VIG can be considered for use in patients with severe ocular vaccinia, but it may increase the risk of corneal scarring.17,23
Progressive vaccinia (a.k.a. vaccinia necrosum, vaccinia gangrenosum) is defined as an uncontrolled replication of vaccinia virus at the vaccination site that leads to a slow and progressive necrosis of surrounding tissue.24 Satellite necrotic lesions typically develop, and ultimately vaccinia virus may be found in other tissues and organs.24 This condition typically affects individuals with incompetent immune systems.24,25 The cardinal clinical signs of progressive vaccinia include an unhealed vaccination site >15 days post vaccination, and the lack of inflammation or an immune response at the vaccination site.24,25 Untreated progressive vaccinia is fatal, but treatment with VIG or the antiviral cidofovir may be effective in some cases.24,25 VIG and thiosemicarbazone treatment in the late 1960s and 1970s reduced the fatality rate for progressive vaccinia from near 100% to 33%.23,25,26 Surgical debridement or amputation may also provide some benefit.24, 25
Eczema vaccinatum is a cutaneous dissemination of vaccinia virus that usually occurs in persons with pre-existing skin disease. It is typically mild and self-limited, but it may be severe or fatal, especially in young children. Death is usually caused by extensive viral dissemination, fluid and electrolyte imbalance, and bacterial sepsis.25,27 Treatment with VIG or antivirals may be effective in some cases.25 Supportive care used for burn victims may help retain proper fluid and electrolyte balance and reduce mortality from eczema vaccinatum.2 Improvements in intensive care therapy during the 1960s likely contributed to the lowering of the fatality rate for eczema vaccinatum from 10% to 1% to 2%.26,27
Post-vaccinial encephalitis is a rare adverse event that frequently leads to death, especially in infants and young children. Reported case fatality rates range from 9% to 40%.25,28 Ten to twenty-five percent of surviving patients have permanent neurologic sequelae.25,28 No predisposing conditions have been identified for this condition, and treatment with VIG has little to no effect.21,23,25
Generalized vaccinia results from blood-borne dissemination of vaccinia virus.23,25 Patients affected with this condition have a generalized rash that is typically self-limited and requires no therapy. VIG can be administered to speed recovery.23,25 This condition may occur in immunosuppressed individuals, but it can also affect those without any underlying illness or risk factors.25
Comments
Post a Comment